In this article published in the December 7, 2018 issue of BenefitsPRO, Sutter Health Plus Vice President of Sales Rob Carnaroli explains how brokers can recognize market demands to pair clients and their employees with the best health plan options available.
From the rush of open enrollment to keeping pace in an ever-changing industry, brokers are constantly on the move. Connecting clients with the right benefit options come from a deep understanding of emerging trends, new entrants, regional considerations, and marketplace dynamics. Yet, the ability to best serve clients all comes down to one important question: What do consumers want from a health plan?
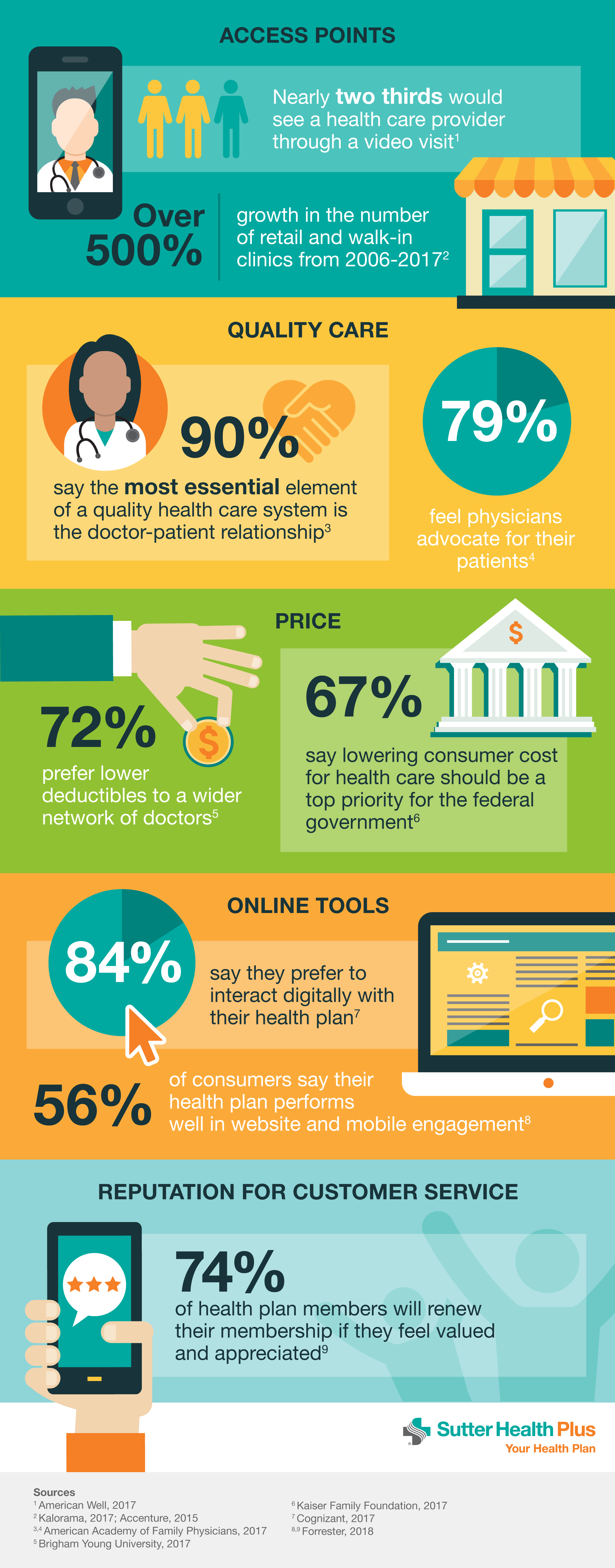
We reviewed data on consumer preferences in health care. After citing multiple studies from elite organizations including the American Academy of Family Physicians, Brigham Young University, and the Kaiser Family Foundation, five core fundamentals stand out: convenient access points, quality care, affordability, easy-to-use online tools, and member-centric customer service.
For brokers, recognizing these market demands can go a long way in pairing a client and their employees with the best health plan options available. Let’s examine each one.
Access points Nearly two-thirds of consumers would consider seeing a healthcare provider through a video visit, according to a 2017 American Well survey. Telemedicine technology appeals to varying demographics. Think of a rural resident far removed from the nearest available clinic, or an urban professional whose doctor visits get derailed by traffic and parking hassles. Communicating with a doctor by smartphone, laptop or tablet can often meet a person’s immediate needs, literally, where they are.
On the brick-and-mortar side, retail clinics are in high demand across the nation. The number of these clinics — where consumers receive everyday primary care services like immunizations and treatment for minor illnesses — increased over 500 percent between 2006 and 2017, according to a recent Kalorama study.
Quality care When consumers choose a healthcare team, relationships matter. According to a 2017 study by the American Academy of Family Physicians, 90 percent of consumers say the most essential element of a quality healthcare system is the doctor-patient relationship. Because people want their doctors to truly care and advocate on their behalf, HMO plans represent a strong option in today’s market. The structure of HMO plans centers on a primary care physician (PCP) partnering with patients to manage most aspects of care, including referrals and care decisions.
In the same survey, 95 percent of consumers were somewhat or very satisfied with their overall relationship with their physician, and 80 percent said they had thought very little or not at all about changing physicians. This speaks volumes about the importance of strong doctor/patient relationships and offering clients a network of providers with a proven record of quality.
Price A 2017 Brigham Young University study stated that 72 percent of consumers polled would prefer a lower deductible versus a wider network of doctors. This indicates that cost is a deciding factor for about three-quarters of health plan shoppers. When developing health plan offerings for clients, the majority of options should continue promoting low deductibles, with a small selection of more robust plans with additional benefits.
Online tools Americans embrace online technology to manage many aspects of their health care. A 2016 Cognizant poll revealed 84 percent of consumers preferred to interact digitally with their health plans. But two years later, only 56 percent of consumers said their health plans perform well on website and mobile management, according to a 2018 Forrester study. Right now, there’s a big gap between what consumers want and what they are experiencing in the digital arena. From member portals to secure messaging with a care team, brokers should play a crucial role in researching and educating clients on accessing each health plan’s online offerings.
Customer service Attention to the customer is vital in any service-based environment, and health care is no different. Forrester’s 2018 study states that 74 percent of health plan members will renew their membership if they feel valued and appreciated. A member’s interactions with customer service staff shape the sentiment for the health plan experience, the study concluded. How resolutely the health plan resolves common issues — benefit, claims, and eligibility inquiries, for example — determines the strength of this emotional connection. Brokers should ask carriers to define their member experience and illustrate what sets them apart in the market.
Conclusion We live in a fast-moving, hyper-connected world. The same technology that seems to make our lives busier also drives healthy innovation and accessibility. Integrated care, concierge service, same-day in-person and virtual solutions for everyday health needs and 24/7 digital access are not projections for the future — it’s all available right here, right now.
By staying in front of consumer trends and expectations, brokers can direct clients to the best coverage for their dollars spent, including new ways to access quality care and convenient service — and showcase their expertise in the marketplace.